Morphine in Myocardial Infarction: Delay in Platelet Inhibition due to Morphine Administered to Patients Presenting with Acute Coronary Syndrome
ABSTRACT
Background:The American College of Cardiology Foundation/American Heart Association Task Force recommends morphine for patients with ST-elevation myocardial infarction and for patients undergoing primary percutaneous coronary intervention (PPCI). A drug-to-drug interaction between morphine and the preferred antiplatelets have been studied to determine the adverse effects on such a combination in antiplatelets. There is an increase risk of thrombic events if platelets are not effectively inhibited during PPCI. The primary aim of this systematic review is to clarify which effects exist on the efficacy of antiplatelet from co-administration of morphine in the setting of acute coronary syndrome (ACS). The secondary aim is to determine if the dose or type of the antiplatelet is a means to overcome the effects of morphine or whether the use of morphine use in ACS should be questioned as it could possibly lead to treatment failure.
Methods:An exhaustive search of the available medical literature was conducted using MEDLINE-Ovid, CINAHL, and Web of Science. Keywords included: morphine, myocardial infarction, STEMI, acute coronary syndrome, antiplatelet, prasugrel, ticagrelor, clopidogrel. Relevant articles were assessed using the Grading of Recommendations, Assessment, and Evaluation (GRADE) system.
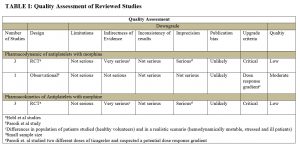
Results: The initial search of databases resulted in 649 studies. Application of eligibility criteria and elimination of duplicates narrowed the search down to 7 studies. With further exclusion criteria applied, 4 studies remained. Three of the remaining studies were randomized, double-blind, placebo-controlled, cross-over trials. One final study was a patient-level integrated analysis. The antiplatelets focused on in the studies were: clopidogrel, ticagrelor, and prasugrel. All 4 studies showed an impact of morphine on the pharmacodynamics of each platelet and the pharmacokinetics of some of the antiplatelets.
Conclusion: Morphine co-administered with antiplatelets in patients with STEMI has the potential to diminish the effects of specific P2Y12 inhibitors. Morphine diminishes pharmacodynamic effects in all recommended antiplatelets and diminishes pharmacokinetics in certain antiplatelets as well. As emerging evidence continues to show the negative impacts of morphine in patients with ACS, clinicians need to be judicious in their use of morphine when co-administered with an antiplatelet.
Keywords: Morphine, antiplatelet, clopidogrel, ticagrelor, prasugrel, acute coronary syndrome, PPCI, myocardial infarction, STEMI
(Click on image to enlarge.)
REVIEWED STUDIES:
Parodi G, Bellandi B, Xanthopoulou I, et al. Morphine is associated with a delayed activity of oral antiplatelet agents in patients with ST-elevation acute myocardial infarction undergoing primary percutaneous coronary intervention. Circulation: Cardiovascular Interventions. 2015;8.
Hobl E, Stimpfl T, Ebner J, et al. Morphine Decreases Clopidogrel Concentrations and Effects A Randomized, Double-Blind, Placebo-Controlled Trial. J Am Coll Cardiol. 2014;63:630-635.
Hobl E, Reiter B, Schoergenhofer C, et al. Morphine decreases ticagrelor concentrations but not its antiplatelet effects: a randomized trial in healthy volunteers. Eur J Clin Invest. 2016;46:7-14.
Hobl E, Reiter B, Schoergenhofer C, et al. Morphine interaction with prasugrel: a double-blind, cross-over trial in healthy volunteers. Clin res cardiol. 2016;105:349-355.
AUTHOR: Stacy Joyce is currently completing her second year in the School of PA Studies at Pacific University, Oregon. She will graduate with an MS degree in August, 2016.

No Comments Yet