Default Options and their Effect on Patients’ Advance Directives
Abstract
Background: Advance directives (ADs) are a way for patients to state their wishes for care in the case that they are unable to express them. Within the US healthcare system, in the absence of ADs or other legal orders, the default is often to sustain life until no longer medically possible. This systematic review analyzes studies that seek to learn how patients >50 years old make decisions for their care on ADs and if default options on the AD form itself could affect their choices.
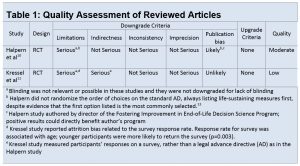
Methods: Exhaustive search of MEDLINE-PubMed, CINAHL, and Web of Science, using the terms “advance directive” and “default.” Relevant studies were assessed for quality using the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) tool.
Results: Two randomized control trials met eligibility criteria. One trial randomly assigned 3 versions of real ADs to seriously ill patients >50 years old. One trial version had a comfort-care default, the other trial had a life-extending care default, and the third was a standard AD control without default options. The other trial randomly assigned 3 versions of surveys about ADs to patients >65 years old. The 3 groups were similar, with an implicit comfort-care default, an implicit life-extension default, and a control without a default. Both studies found that default options affected the way that patients made choices for end-of-life care.
Conclusion: Patient’s decisions for end-of-life care may be affected by default options. Providers, healthcare systems, and states must be aware of this phenomenon when structuring forms and conversations around this subject.
Keywords: Advance directive, default
(Click on image to enlarge.)
REVIEWED STUDIES:
Halpern SD, Loewenstein G, Volpp KG, et al. Default Options In Advance Directives Influence How Patients Set Goals For End-Of-Life Care. Health Affairs. 2013;32(2):408-417. doi:10.1377/hlthaff.2012.0895.
Kressel LM, Chapman GB, Leventhal E. The Influence of Default Options on the Expression of End-of-Life Treatment Preferences in Advance Directives. J GEN INTERN MED Journal of General Internal Medicine. 2007;22(7):1007-1010. doi:10.1007/s11606-007-0204-6.
AUTHOR: Danielle F. Bendicksen graduated from Pacific University, School of PA Studies with an MS degree in August 2017.


No Comments Yet